General Rehabilitation
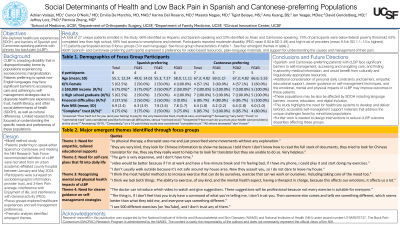
Social Determinants of Health and Low Back Pain Outcomes in Spanish and Cantonese-preferring Populations
Saturday, October 25, 2025
8:00 AM - 9:15 AM MT
Location: Original Research Theater
Has Audio

Adrian Vallejo, MD
Resident
UCSF Health
San Francisco, California
Patricia Zheng, MD
Associate Professor
University of California San Francisco
San Carlos, California
Primary Author(s)
Co-Author(s)
Disclosure(s):
Adrian Vallejo, MD: No financial relationships to disclose
Patricia Zheng, MD: No financial relationships to disclose
Design: Mixed method study; survey and focus group qualitative analysis.
Setting : Urban academic-affiliated county hospital.
Participants : Patients preferring to speak Spanish or Cantonese and meeting the NIH Research Task Force recommended definition of cLBP were recruited between March and May 2024.
Interventions: Participants were surveyed and participated in focus groups conducted in each language probing on healthcare experiences and self-management preferences. Interviews were transcribed and thematically analyzed.
Main Outcome Measures: Sociodemographic information, provider trust, 3-Item Pain average, interference with Enjoyment of life, and interference with General activity (PEG) scores, and emergent themes.
Results: Of 27 total enrolled patients (18 female),18 (66%) identified as Hispanic and Spanish-speaking, 9 (33%) identified as Asian and Cantonese-speaking, 75% were below federal poverty threshold, 63% completed less than high school, and 59% had access to smartphone and internet. Participants reported moderate disability (PEG mean 6.82±SD 2.49) and high provider trust (mean 9.5± SD 1.1; 10 is highest).
Of 15 focus group participants, 8 (53%) identified as Hispanic and Spanish-speaking with mean age 55.1 (SD 12.2) years, and 7 (47%) identified as Asian and Cantonese-speaking with mean age 69.0 (SD 2.0) years.
Four themes emerged: 1) need for empathic, tailored educational supports, 2) desire for self-management plans accounting for social and economic constraints, 3) recognition of mental health and social isolation influencing cLBP experience, and 4) need for clearer guidance on self-management strategies and trustworthy resources.
Conclusions: Spanish and Cantonese-preferring patients with cLBP face significant barriers to self-management and accessing and navigating care. Consideration of these barriers in practice, further work, and clinical interventions may improve outcomes in these patients.

.jpg)