Neurological Rehabilitation
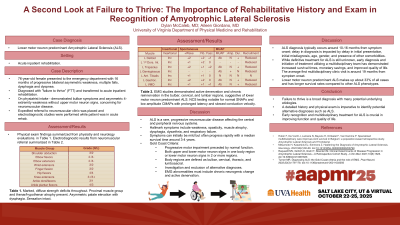
A Second Look at Failure to Thrive: The Importance of Rehabilitative History and Exam in Recognition of Amyotrophic Lateral Sclerosis
Thursday, October 23, 2025
12:45 PM - 2:15 PM MT
Location: Kiosk 6
Has Audio
Dylan McCaleb, MD (he/him/his)
Resident Physician
University of Virginia Medical Center PM&R Program
Charlottesville, Virginia- AG
Aileen Giordano, MD
Assistant Professor
Aileen Giordano MD
Crozet, Virginia
Primary Author(s)
Co-Author(s)
Disclosure(s):
Dylan McCaleb, MD: No financial relationships to disclose
Case Description or Program Description: A 76-year-old female presented to the emergency department with 16 months of progressive bilateral asymmetric weakness with subsequent increase in falls and onset of dysphagia and dyspnea. No further workup into neurologic symptoms was pursued and she was transferred to acute inpatient rehabilitation for "failure to thrive" (FTT). On initial physiatrist evaluation, the patient demonstrated bulbar symptoms and asymmetric 4-extremity weakness without upper motor neuron signs, concerning for neuromuscular disease. The physiatrist placed an expedited referral to neurology and ordered electrodiagnostic studies.
Setting: Acute inpatient rehabilitation.
Assessment/Results: Electrodiagnostic studies demonstrated active denervation and chronic reinnervation in the bulbar, cervical, and lumbar regions, suggestive of lower motor neuron predominant amyotrophic lateral sclerosis. The patient was functionally optimized in acute inpatient rehabilitation and transitioned to an outpatient ALS multidisciplinary clinic for follow-up care.
Discussion (relevance): ALS is a rare, progressive neuromuscular disease affecting the central and peripheral nervous systems. Hallmark symptoms include weakness, spasticity, muscle atrophy, dysphagia, dysarthria, and eventually respiratory failure. Symptoms can initially be mild but often progress rapidly with a median survival time around 3 to 4 years. Furthermore, ALS diagnosis typically occurs around 10-16 months from symptom onset; delay in diagnosis is impacted by delay in initial presentation, initial misdiagnosis, age, and presence of other comorbidities. While definitive treatment for ALS is still unknown, early diagnosis and initiation of treatment utilizing a multidisciplinary team has demonstrated increased survival times, monetary savings, and improved quality of life.
Conclusions: Failure to thrive is a broad diagnosis with many potential underlying etiologies. When evaluating FTT patients, a detailed history and physical exam is imperative to identify potential alternative diagnoses like ALS. Early recognition of ALS is crucial in improving function and quality of life.

.jpg)