Neurological Rehabilitation
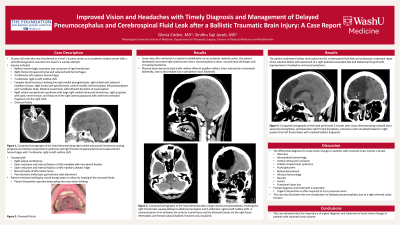
Improved Vision and Headaches with Timely Diagnosis and Management of Delayed Pneumocephalus and Cerebrospinal Fluid Leak after a Ballistic Traumatic Brain Injury: A Case Report
Thursday, October 23, 2025
12:45 PM - 2:15 PM MT
Location: Kiosk 5

Gloria Coden, MD
PGY-2
Washington University/B-JH/SLCH Consortium PM&R Program
Saint Louis, Missouri- SJ
Sindhu S. Jacob, MD
Associate Professor
Washington University in Saint Louis
Saint Louis, Missouri
Primary Author(s)
Co-Author(s)
Disclosure(s):
Gloria Coden, MD: No financial relationships to disclose
Case Description or Program Description: 26-year-old male presented with a self-inflicted gunshot wound to the head in a suicide attempt. Injuries included bilateral subarachnoid, right frontal intraparenchymal, bilateral temporal subdural hemorrhages, 7-millimeter right-to-left midline shift, multiple facial fractures, right retrobulbar hemorrhage with orbital compartment syndrome, and oronasal fistula which was treated with a right lateral canthotomy and open reduction and internal fixation. Seven days after admission to inpatient rehabilitation, the patient developed new-onset right-sided tunnel vision, worsening blurry vision, mucoid nasal discharge, and increasing headaches. Physical exam demonstrated no discernable loss in peripheral vision bilaterally.
Setting: Inpatient rehabilitation at an academic medical center
Assessment/Results: Computed tomography of the head demonstrated a large volume pneumocephalus involving the right frontal lobe causing leftward subfalcine herniation and 5-millimeter right-to-left midline shift. A communication of air between the anterior cranial fossa and the ethmoid sinuses via the right fovea ethmoidalis and frontal calvarial ballistic fractures was visualized. The patient underwent lumbar drain placement for cerebrospinal fluid leak and endoscopic endonasal repair of the calvarial defect with placement of a right pedicled nasoseptal flap and abdominal fat graft with improvement in headaches and visual symptoms.
Discussion (relevance): The differential diagnosis for acute vision changes in patients with traumatic brain injuries is broad, including infarction, intracerebral hemorrhage, central retinal vein occlusion, orbital compartment syndrome, acute glaucoma, retinal detachment, vitreous hemorrhage, neuritis, uveitis, and functional vision loss. Prompt diagnosis and treatment is important, as urgent intervention is often required to try to preserve vision. This case also illustrates the rare complication of delayed pneumocephalus due to a right ethmoid cavity fracture.
Conclusions: This case demonstrates the importance of urgent diagnosis and treatment of acute vision changes in patients with traumatic brain injuries.

.jpg)