General Rehabilitation
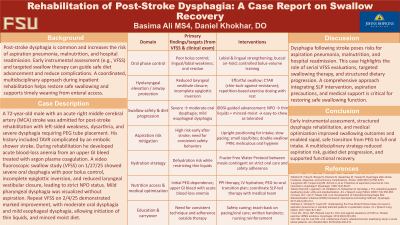
Rehabilitation of Post-Stroke Dysphagia: A Case Report on Swallow Recovery
Thursday, October 23, 2025
5:00 PM - 6:30 PM MT
Location: Open Kiosks
.jpg)
Basima Ali
Medical Student
Florida State University College of Medicine
Land O Lakes, Florida
Daniel Khokhar, DO
Resident
Johns Hopkins PM&R
Baltimore, Maryland
Poster Presenter(s)
Co-Author(s)
Disclosure(s):
Basima Ali: No financial relationships to disclose
Daniel Khokhar, DO: No financial relationships to disclose
Case Description or Program Description: The patient was admitted for post-stroke rehabilitation with left-sided weakness, dysarthria, and severe dysphagia requiring PEG tube placement. His history included TAVR complicated by an embolic shower stroke. During rehabilitation, he developed acute blood loss anemia due to an upper gastrointestinal bleed, which was treated with argon plasma coagulation.
A videofluoroscopic swallow study (VFSS) on 1/27/25 revealed severe oral dysphagia with poor bolus control, incomplete epiglottic inversion, and reduced laryngeal vestibular closure, leading to strict NPO status. Mild pharyngeal dysphagia was present, though no aspiration was observed. A repeat VFSS on 2/4/25 demonstrated marked improvement, with moderate oral dysphagia and mild esophageal dysphagia, allowing initiation of thin liquids, and minced moist diet.
Setting: Acute inpatient rehabilitation facility.
Assessment/Results: A multidisciplinary rehabilitation approach was implemented, including:
• Oral motor exercises (labial and lingual strengthening, buccal air hold).
• Swallow strengthening exercises (effortful swallow, chin tuck against resistance).
• Dietary modifications (texture progression from minced moist to easy-to-chew foods).
• Aspiration precautions (upright positioning, slow-paced intake, oral hygiene).
• Frazier Free Water Protocol (permitting water after stringent oral care).
• Medical optimization (IV hydration, proton pump inhibitor therapy, PEG tube weaning).
By 2/21/25, the patient demonstrated safe oral intake without aspiration and was successfully transitioned from PEG tube dependence to full oral nutrition.
Discussion (relevance): Dysphagia following stroke poses risks for aspiration pneumonia, malnutrition, and hospital readmission. This case highlights the role of serial VFSS evaluations, targeted swallowing therapy, and structured dietary progression. A comprehensive approach integrating SLP intervention, aspiration precautions, and medical support is critical for restoring safe swallowing function.
Conclusions: Early dysphagia assessment, structured rehabilitation, and medical optimization significantly improve post-stroke swallowing outcomes. A multidisciplinary strategy is essential to reduce aspiration risk, facilitate diet progression, and enhance patient recovery.

.jpg)