General Rehabilitation
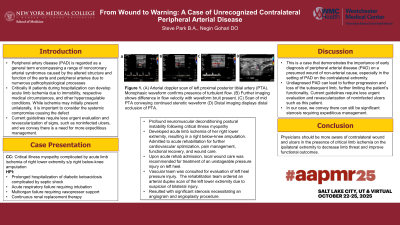
From Wound to Warning: A Case of Unrecognized Contralateral Peripheral Arterial Disease
Saturday, October 25, 2025
12:00 PM - 1:30 PM MT
Location: Kiosk 2
.jpg)
Steve Park, Other (he/him/his)
Medical Student
New York Medical College
Las Vegas, Nevada- NG
Negin Gohari, DO
Clinical Associate Professor
Hofstra Northwell School of Medicine PM&R Program
Great Neck, New York
Poster Presenter(s)
Co-Author(s)
Disclosure(s):
Steve Park, Other: No financial relationships to disclose
Case Description or Program Description: During the hospitalization, patient developed acute limb ischemia of her right lower extremity, resulting in a right below-knee amputation. Post-operatively, patient was transferred to acute inpatient rehabilitation for further cardiovascular optimization, pain management, functional recovery, and wound care.
Setting: Acute inpatient rehabilitation at quaternary care hospital
Assessment/Results: Upon her discharge from the acute care hospital, local wound care was recommended for treatment of an unstageable pressure injury on left heel. Upon acute rehab admission, vascular team was consulted for evaluation of left heel pressure injury. The rehabilitation team ordered an arterial duplex scan of the left lower extremity, which resulted with significant stenosis necessitating an angiogram and angioplasty procedure.
Discussion (relevance): This is a case that demonstrates the importance of early diagnosis of peripheral arterial disease (PAD) on a presumed wound of non-arterial cause, especially in the setting of PAD on the contralateral extremity. Undiagnosed PAD can lead to further progression and loss of the subsequent limb, further limiting the patient’s functionality. Current guidelines require less urgent evaluation and revascularization of noninfected ulcers such as this patient's. In our case, we convey there can still be significant stenosis requiring expeditious management.
Conclusions: Physicians should be more aware of contralateral wound and ulcers in the presence of critical limb ischemia on the ipsilateral extremity to decrease limb threat and improve functional outcomes.

.jpg)