Neurological Rehabilitation
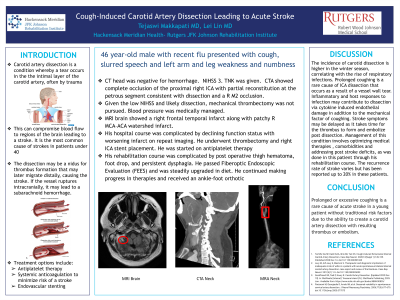
Cough-Induced Carotid Artery Dissection Leading to Acute Stroke
Saturday, October 25, 2025
8:00 AM - 9:15 AM MT
Location: Kiosk 5
- LL
Lei Lin, MD, PhD
Associate Professor
JFK Johnson Rehabilitation Institute
Edison, New Jersey 
Teja Makkapati, MD
Resident
JFK Medical Center PM&R Program
Edison, New Jersey
Co-Author(s)
Poster Presenter(s)
Disclosure(s):
Teja Makkapati, MD: No financial relationships to disclose
Case Description or Program Description: 46-year-old male with medical history notable for flu with severe coughing presented with slurred speech and arm weakness. Patient received Tenecteplase. Angiography showed complete occlusion of the proximal right internal carotid artery (ICA) with partial reconstitution consistent with dissection and a right middle cerebral artery occlusion. Patient underwent carotid artery stenting with interventional radiology and started on dual antiplatelet therapy and transferred to IRF. The rehabilitation course was complicated by management of dysphagia, new-onset prediabetes and foot drop.
Setting: inpatient acute rehabilitation hospital
Assessment/Results: At 2 weeks post admission to IRF, the patient tolerated a comprehensive rehabilitation program. His therapists noted continued improvements in coordination and dysphagia. He was evaluated for an ankle-foot-orthosis to help with foot drop. His sleeping and eating both significantly improved. Further developments will be discussed.
Discussion (relevance): Prolonged coughing is a rare cause of ICA dissection that occurs as a result of a vessel wall tear, leading to thrombosis. This can also result in embolism, thus causing an acute ischemic stroke. Stroke symptoms may be delayed as it takes time for the thrombus to form and embolize post dissection. Management of this condition involves optimizing medical therapies and comorbidities, as was done in this patient through his rehabilitation course.
Conclusions: We describe a unique case of an acute ischemic infarct that was a result of a cough induced carotid artery dissection.

.jpg)