Pain and Spine Medicine
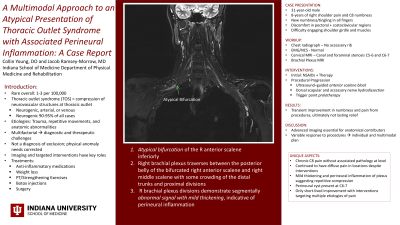
A Multimodal Approach to an Atypical Presentation of Thoracic Outlet Syndrome with Associated Perineural Inflammation: A Case Report
Friday, October 24, 2025
12:00 PM - 1:30 PM MT
Location: Kiosk 4

Collin M. Young, DO
Resident Physician
Indiana University School of Medicine PM&R Program
Indianapolis, Indiana
Poster Presenter(s)
Disclosure(s):
Collin M. Young, DO: No financial relationships to disclose
Case Description or Program Description: Patient is a 31 year-old male without significant past medical history or trauma with chronic right shoulder pain and radiating symptoms.
Setting: Outpatient Neuromuscular/Spine Consult
Assessment/Results: A 31-year-old male presented with an eight-year history of right shoulder pain radiating to the fifth finger, worsening over days prior to initial encounter with new numbness and tingling in all fingers. He reported difficulty engaging shoulder girdle muscles and discomfort in the pectoral and costoclavicular regions. Examination revealed mild cervical range of motion limitations, tenderness over the right scalenes and pectoralis muscle, and right C8 hypoesthesia. Initial imaging showed mild cervical degenerative changes without significant foraminal stenosis. EMG was normal. Brachial plexus MRI demonstrated an atypical bifurcation of the right anterior scalene, brachial plexus crowding, and segmental perineural inflammation suggestive of repetitive impingement. Conservative treatments, including NSAIDs and manual therapy, provided minimal relief. The patient underwent ultrasound-guided anterior scalene muscle block, followed by dorsal scapular and accessory nerve hydrodissection with trigger point prolotherapy. He reported initial symptom relief but experienced recurrence, leading to consideration of an epidural steroid injection even in the setting of mild cervical imaging findings.
Discussion (relevance): This case underscores the importance of advanced imaging in identifying anatomical contributors to TOS. The patient’s partial response to injections highlights the variability in treatment outcomes and the need for individualized management.
Conclusions: TOS remains a diagnostic and therapeutic challenge due to its multifactorial nature. This case illustrates the role of multimodal interventions in addressing structural and inflammatory contributors to symptoms. While nerve hydrodissection and prolotherapy offered temporary relief, recurrence suggests the need for further research to optimize long-term management strategies.

.jpg)